Introduction
Mental health dysfunctions are on the rise, with every 1 in 5 adults experiencing mental illness every year, with suicide being one of the leading causes of death among people across various age groups. [1] Our mental health is deteriorating because the reality we live in is less than ideal. Social inequality, war and injustice, economic uncertainties, the pressure to conform to the unrealistic expectations of society, and the further distortion of reality by social media have become the norm. A deep-rooted cultural stigma around mental health discourages us from seeking the support we need. On top of this, mental disorders and complex symptoms often overlap, which can make it more challenging to diagnose and treat them correctly. The need of the hour is evidence-based approaches as they are developed through rigorous clinical trials and tested and continuously evaluated for their efficacy. For the scope of this blog, we’ll dive into cognitive behavioral therapy (CBT) and dialectical behavioral therapy (DBT) as they are effective in addressing a wide range of mental health conditions today. Let’s understand these psychotherapies, the differences between CBT vs. DBT, their similarities, and which one is right for you.
Define CBT and DBT
Cognitive behavioral therapy functions on the principle that beliefs and thoughts result in certain emotions, which result in the way we act and react, which further reinforces our beliefs. Hence, if we have a negative thought about ourselves, someone else, or a situation, it will only intensify through our emotions, leading to unfavorable behavior and outcomes.[2] Through CBT, we can learn to identify and challenge the thought patterns that are not serving us and replace them with more realistic and positive thoughts that can help us achieve our goals.
Dr Marsha Linehan developed dialectical behavior therapy, which was first used to treat borderline personality disorder (BPD). The philosophy behind DBT is to integrate opposing views to strike a balance. Sometimes known as talk therapy, DBT is also based on cognitive-behavioral principles and is structured into four main components- group skills training, individual psychotherapy, telephone consultation, and therapist consultation team.[3] Together, these components are aimed at teaching you behavioral skills, namely mindfulness, emotional regulation, distress tolerance, and interpersonal effectiveness, which can help you manage your symptoms.
Difference Between CBT Vs DBT
The key differences between CBT and DBT are the philosophy they’re based on, their approach to treatment and techniques used, and what they’re targeted to treat.
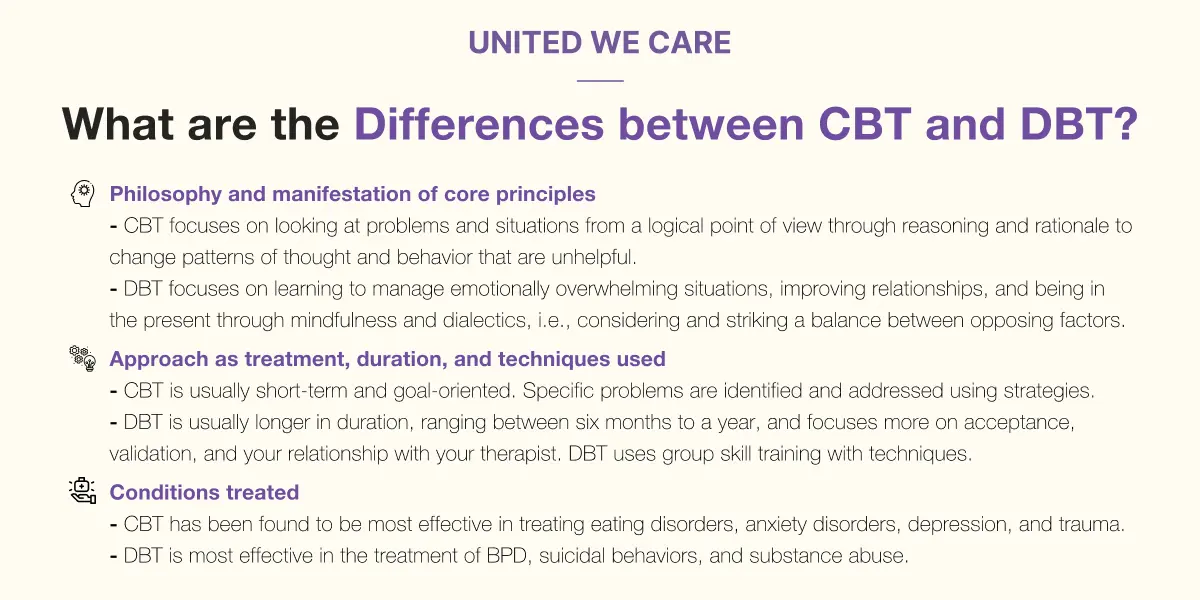
Philosophy and manifestation of core principles
CBT focuses on looking at problems and situations from a logical point of view through reasoning and rationale to change patterns of thought and behavior that are unhelpful.
DBT, on the other hand, focuses primarily on accepting things the way they are while simultaneously working towards change. DBT focuses on learning to manage emotionally overwhelming situations, improving relationships, and being in the present through mindfulness and dialectics, i.e., considering and striking a balance between opposing factors. The Eastern philosophies of Zen and Buddhism influence these concepts.
Approach as treatment, duration, and techniques used
CBT is usually short-term and goal-oriented. Specific problems are identified and addressed using strategies such as:
- Cognitive restructuring: Challenging negative thoughts by looking for evidence to support them and, in the absence of proof, replacing these thoughts with balanced and positive narratives.
- Exposure therapy: Confronting your fears and phobias and learning to cope with them by gradually exposing yourself to them in a clinically controlled setting.
- Relaxation and stress reduction: Practicing deep breathing, guided imagery, or progressive muscle relaxation to lower your stress and anxiety.
DBT is usually longer in duration, ranging between six months to a year, and focuses more on acceptance, validation, and your relationship with your therapist. DBT uses group skill training with techniques such as [4]
- Mindfulness meditation: Learning to reach and maintain a balanced state of mind by not judging anything to be good or bad.
- Emotional regulation: Identifying your intense emotion and managing it by acting in the opposite way of your urges so that you can respond in a healthy and non-destructive way.
- Distress tolerance: Activating yourself on a physiological level to be able to tolerate and survive distressing situations without impulsively engaging in risky behavior such as self-harm. You can do this by immersing your face in ice-cold water or engaging in paced breathing.
- Interpersonal effectiveness skills: Communicating your needs with clarity and assertiveness, helping you manage conflict and have better relationships with people.
Conditions treated
CBT has been found to be most effective in treating eating disorders, anxiety disorders, depression, and trauma. DBT is most effective in the treatment of BPD, suicidal behaviors, and substance abuse.
Similarities between CBT and DBT
Cognitive behavioral therapy and dialectical behavioral therapy are both evidence-based psychotherapies with key similarities such as:
- Having roots in cognitive behavioral theory: Both therapies recognize the interconnection between our thoughts, emotions, and behaviors and focus on the development of coping skills to deal with unhealthy behavior.
- Psychoeducating clients: Clients are empowered and given education on their mental health, the process of the therapy, and specific skills they can use to cope.
- Effectiveness: Both CBT and DBT are widely recognized and effective in the treatment of various conditions. A 2019 study explored the benefits of CBT for 124 adults undergoing 12 weeks of group CBT. The results suggested that CBT is equally effective in treating depression, anxiety, and executive and social functioning. [5] A 2022 study explored the effectiveness of 6 months of DBT on patients with BPD. The results suggest that DBT can effectively reduce tendencies of self-harm and improve coping skills in the participants. [6]
- Professional as well as self-help support in digital format: It is possible to use digital platforms and tools for online therapy as well as self-help, such as tracking mood and behavior.
Conclusion
CBT and DBT are evidence-based psychotherapies that are effective in the treatment of a wide range of mental health conditions such as depression, anxiety disorders, and eating disorders through CBT and BPD and suicidal behavior through DBT. The key differences between these therapies are the philosophy they’re influenced by, their approach to treatment, the duration and techniques used, and the conditions treated. However, their similarity lies in the fact that both are rooted in cognitive behavioral theory with an emphasis on the relationship between thoughts, emotions, and behavior, along with other similarities such as focus on the psychoeducation of clients and adaptability in digital format.
Which therapy is better suited for you is best decided by a mental health professional who will examine your history and symptoms and suggest a therapy option based on your unique needs. Book a session with one of our mental health experts, who can help you understand whether CBT or DBT is more appropriate for you. At United We Care, we offer the most suitable, clinically backed solutions for all your needs for well-being.
References:
[1] National Alliance on Mental Illness, “Mental Health By the Numbers,” NAMI. [Online]. Available: https://nami.org/mhstats?gclid=Cj0KCQiA7bucBhCeARIsAIOwr-_mryPgVr3hp8Lz9-i-aijtm5GJWQeY_Q8IM0faz9DI722oo2Q2TFAaAjFGEALw_wcB. Accessed: Nov. 29, 2023.
[2] Steven C. Hayes, Stefan G. Hofmann, Process-Based CBT: The Science and Core Clinical Competencies of Cognitive Behavioral Therapy. [Online]. Available: https://books.google.co.in/books?id=J0tHDgAAQBAJ. Accessed: Nov. 29, 2023.
[3] J. M. May, T. M. Richards, and K. S. Barth, “Dialectical behavior therapy as a treatment for borderline personality disorder,” The Mental Health Clinician, vol. 6, no. 2, pp. 62–67, 2016. [Online]. Available: https://doi.org/10.9740/mhc.2016.03.62. Accessed: Nov. 29, 2023.
[4] Jennifer M May, MD; Toni M Richardi, PsyD; Kelly S Barth, DO, “Dialectical behavior therapy as a treatment for borderline personality disorder in The Mental Health Clinician, vol. 6, no. 2. [Online]. Available: https://meridian.allenpress.com/mhc/article/6/2/62/127854/Dialectical-behavior-therapy-as-treatment-for. Accessed: Nov. 29, 2023.
[5] M.-R. Pan et al., “A comparison of efficacy between cognitive behavioral therapy (CBT) and CBT combined with medication in adults with attention-deficit/hyperactivity disorder (ADHD),” Psychiatry Research, vol. 279, pp. 23–33, 2019. [Online]. Available: https://doi.org/10.1016/j.psychres.2019.06.040. Accessed: Nov. 29, 2023.
[6] Shelley F. McMain; Alexander L. Chapman; Janice R. Kuo; Katherine L. Dixon-Gordon; Timothy Henry Guimond; Cathy Labrish; Wanrudee Isaranuwatchai; David L. Streiner, “The Effectiveness of 6 versus 12 Months of Dialectical Behavior Therapy for Borderline Personality Disorder: A Noninferiority Randomized Clinical Trial,” in Psychotherapy and Psychosomatics, vol. 91, no. 6: 382–397, 2022. [Online]. Available: https://karger.com/pps/article/91/6/382/826589/The-Effectiveness-of-6-versus-12. Accessed: Nov. 29, 2023.





